A nurse is calculating a client’s fluid intake – In the realm of nursing, accurately calculating a client’s fluid intake is paramount to maintaining optimal health outcomes. This comprehensive guide delves into the intricacies of fluid intake monitoring, empowering nurses with the knowledge and skills to ensure their clients receive appropriate hydration.
Fluid intake calculation is a crucial aspect of nursing practice, providing valuable insights into a client’s overall fluid balance. Accurate monitoring helps identify potential fluid imbalances, prevent dehydration, and guide appropriate interventions to maintain hydration status.
Fluid Intake Calculation in Nursing: A Nurse Is Calculating A Client’s Fluid Intake
Fluid intake calculation is an essential aspect of nursing care, providing valuable insights into a client’s hydration status and overall well-being. Accurate monitoring of fluid intake helps healthcare professionals make informed decisions about fluid management and prevent potential complications.
Definition and Purpose
Fluid intake calculation involves determining the total amount of fluids consumed by a client over a specific period, typically 24 hours. This calculation includes all fluids, regardless of source or route of administration, such as oral fluids, intravenous fluids, and enteral nutrition.
Accurate fluid intake monitoring is crucial for maintaining fluid balance, preventing dehydration, and managing electrolyte levels. It also helps assess a client’s nutritional status, identify fluid shifts, and monitor the effectiveness of fluid replacement therapies.
Methods of Calculation, A nurse is calculating a client’s fluid intake
Fluid intake can be calculated manually or using technology.
- Manual Calculation:This involves measuring and recording the volume of all fluids consumed by the client, including fluids from meals, beverages, medications, and medical devices. A graduated cylinder or other measuring device is used to determine the volume.
- Technology-Assisted Calculation:Electronic health records (EHRs) and other software systems can automate fluid intake calculation. These systems use data from various sources, such as medication administration records, nutritional assessments, and vital signs, to calculate the client’s fluid intake.
Types of Fluids
Fluids included in fluid intake calculations are categorized as follows:
- Oral Fluids:Fluids consumed by mouth, including water, juices, soups, and beverages.
- Intravenous Fluids:Fluids administered directly into a vein, typically through an IV line.
- Enteral Fluids:Fluids delivered into the gastrointestinal tract through a feeding tube or other enteral device.
Distinguishing between oral and intravenous fluids is important because intravenous fluids bypass the digestive system and directly enter the bloodstream.
Factors Influencing Fluid Intake
Several factors can affect a client’s fluid intake, including:
- Age:Infants and elderly adults have higher fluid needs relative to their body weight.
- Medical Conditions:Conditions such as diabetes, renal disease, and heart failure can alter fluid intake and electrolyte balance.
- Medications:Some medications, such as diuretics, can increase fluid loss.
- Environmental Factors:Hot and humid environments increase fluid loss through sweating.
Understanding these factors is essential for tailoring fluid intake calculations to individual client needs.
Documentation and Reporting
Fluid intake data is typically documented in a client’s medical record. Accurate and timely reporting of fluid intake is crucial for:
- Tracking fluid balance and monitoring for dehydration or fluid overload.
- Assessing the effectiveness of fluid replacement therapies.
- Identifying trends in fluid intake that may indicate underlying health issues.
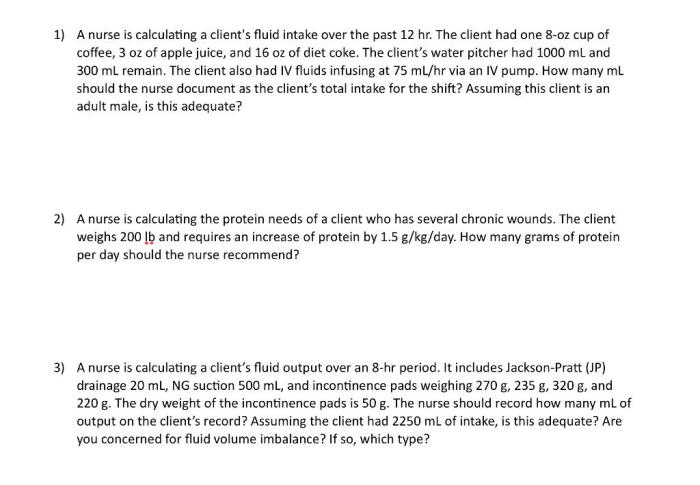
Case Study
A 70-year-old male client with heart failure is admitted to the hospital with shortness of breath and edema. As part of his care plan, his fluid intake is closely monitored.
Over a 24-hour period, the client consumes:
- 8 ounces of water
- 12 ounces of orange juice
- 1 cup of soup
- 1,000 mL of intravenous fluids
Fluid Intake Calculation:
| Fluid Source | Volume |
|---|---|
| Oral Fluids | 8 oz + 12 oz + 1 cup = 32 oz |
| Intravenous Fluids | 1,000 mL |
| Total Fluid Intake | 32 oz + 1,000 mL = 1,332 mL |
The client’s total fluid intake over the 24-hour period is 1,332 mL. This information will be used to guide his fluid management and ensure adequate hydration while preventing fluid overload.
FAQ Section
What is the significance of distinguishing between oral and intravenous fluids in fluid intake calculations?
Oral fluids are consumed through the mouth, while intravenous fluids are administered directly into the bloodstream. This distinction is important because intravenous fluids bypass the gastrointestinal tract and are absorbed directly into the bloodstream, contributing to a client’s fluid balance more rapidly than oral fluids.
How can nurses ensure accurate and timely reporting of fluid intake data?
Nurses can employ various methods to ensure accurate and timely reporting of fluid intake data, including using standardized documentation tools, implementing electronic health records, and conducting regular audits to monitor the accuracy of fluid intake records.